In a groundbreaking move for maternal healthcare, the National Health Service (NHS) in England has announced a pioneering initiative to provide pregnant women with type 1 diabetes access to advanced artificial pancreas systems, also known as hybrid closed-loop systems.
This revolutionary technology aims to significantly reduce the risks of stillbirth, miscarriage, and other adverse pregnancy outcomes by offering precise blood glucose management. This development marks a significant step forward in improving the health and wellbeing of both mothers-to-be and their babies, addressing the unique challenges faced by the approximately 2,000 women with type 1 diabetes who become pregnant each year in England.
Understanding Type 1 Diabetes and Pregnancy Challenges
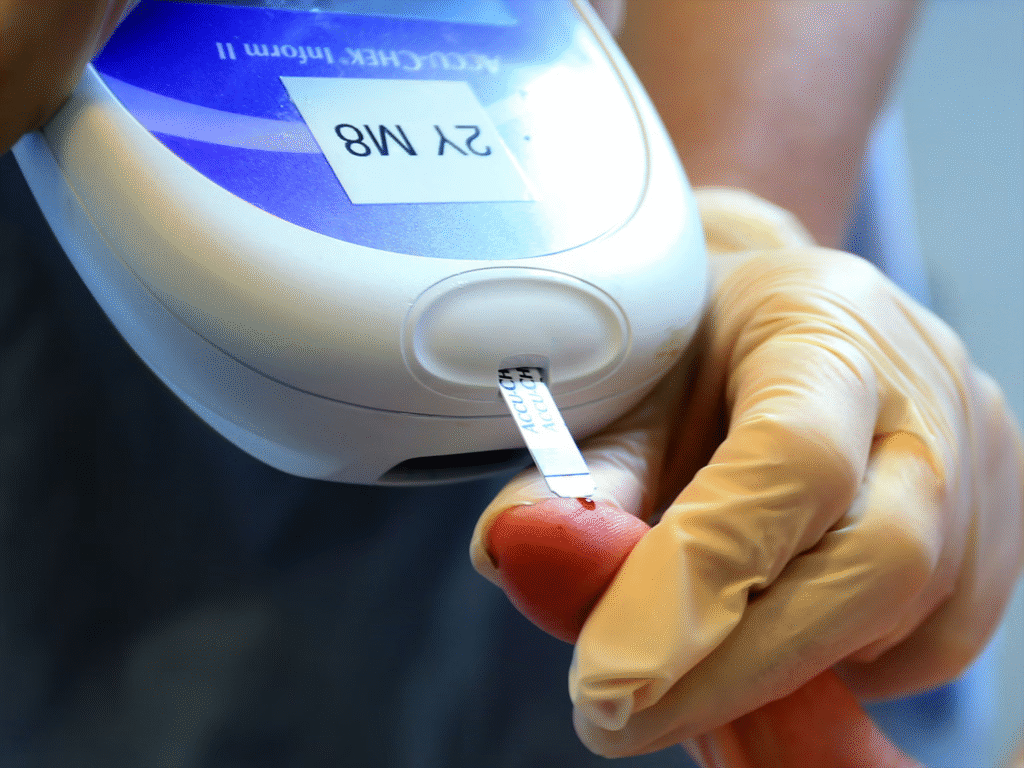
Type 1 diabetes is a lifelong autoimmune condition affecting around 400,000 people in the United Kingdom. It occurs when the immune system attacks insulin-producing cells in the pancreas, leaving the body unable to regulate blood sugar levels naturally. Insulin, a hormone critical for converting sugar into energy, must be administered through injections or pumps, requiring constant monitoring to prevent dangerously high or low blood glucose levels.
For pregnant women, this management becomes even more complex due to hormonal changes during pregnancy, which can make blood glucose levels harder to control. Poorly managed diabetes during pregnancy poses significant risks. Elevated blood sugar levels can lead to serious complications, including stillbirth, miscarriage, larger-than-average babies (macrosomia), birth injuries, and an increased need for neonatal intensive care.
For instance, babies born to mothers with uncontrolled diabetes may face issues such as jaundice, weight problems, or other health complications requiring specialized care. The physical and emotional toll of constant monitoring—often involving hourly finger-prick tests during the day and every 30 minutes overnight—can be overwhelming for expectant mothers.
Thousands of mums-to-be in England living with type 1 diabetes are to receive a pregnancy-specific Hybrid Closed Loop System, also known as an ‘artificial pancreas’, to help them manage their blood glucose levels.
— NHS England (@NHSEngland) September 5, 2025
Read more ➡️ https://t.co/d1mdfQwXmn pic.twitter.com/w8QhTBRyu6
This is exemplified by the experience of Nina Willer, a 40-year-old diabetes specialist midwife from Norwich, who, during her first pregnancy, relied on such intensive manual monitoring, resulting in her daughter needing a week of neonatal intensive care for multiple health issues. The NHS’s initiative to roll out artificial pancreas systems specifically tailored for pregnancy addresses these challenges head-on. By automating blood glucose management, this technology alleviates the burden of constant manual intervention, offering a safer and less stressful pregnancy experience for women with type 1 diabetes.
The Artificial Pancreas: A Game-Changing Technology
The artificial pancreas, or hybrid closed-loop system, is a cutting-edge medical device designed to mimic the function of a healthy pancreas by automatically regulating blood glucose levels. The system comprises three key components: an insulin pump, a continuous glucose monitor (CGM), and an advanced algorithm that operates via a mobile phone app.
The CGM continuously tracks blood glucose levels, sending real-time data to the algorithm, which calculates and delivers precise insulin doses through the pump. Unlike traditional insulin pumps, which require manual adjustments, this system operates 24/7, adjusting insulin delivery dynamically based on the body’s needs.
Read : MedMiracle! Smartphone-Based Diabetes Test Could Diagnose Condition in Under 10 Minutes
What sets this pregnancy-specific artificial pancreas apart is its ability to allow women to set lower glucose targets, which are critical for achieving optimal pregnancy outcomes. Pregnancy requires tighter glucose control to minimize risks to both mother and baby, and this system is uniquely designed to meet those stringent requirements. Additionally, the technology enables remote monitoring by healthcare professionals, reducing the need for frequent in-person check-ups and allowing for more flexible, patient-centered care.

The NHS has already distributed this technology to over 600 pregnant women with type 1 diabetes in the initiative’s first phase, with plans to extend it to all eligible women, including those planning a pregnancy. The system’s effectiveness is underscored by testimonials like that of Nina Willer, who used the artificial pancreas during her second pregnancy. Unlike her first experience, which involved exhaustive manual monitoring, the technology allowed her to achieve better glucose control with less effort, resulting in the birth of a healthy daughter at 36 weeks without the need for intensive neonatal care.
Partha Kar, the Type 1 Diabetes Technology Lead at NHS England, describes the technology as “ingenious yet simple,” emphasizing its ability to improve maternal outcomes, reduce serious health complications, and simplify care. Similarly, Anthony Walker, a senior policy officer at Diabetes UK, highlights the importance of providing hybrid closed-loop systems proven effective for pregnancy, along with necessary devices like mobile phones, to ensure equitable access to this transformative technology.
Impact on Maternal and Neonatal Health Outcomes
The introduction of artificial pancreas systems for pregnant women with type 1 diabetes is poised to have a profound impact on maternal and neonatal health. Effective blood glucose management before and during pregnancy has been shown to significantly reduce the risk of adverse outcomes such as miscarriage, stillbirth, birth injuries, and developmental issues in babies. By automating insulin delivery and maintaining glucose levels within a safe range, the technology minimizes the likelihood of complications that can arise from poorly controlled diabetes.
One of the most significant benefits is the reduction in the physical and mental burden on expectant mothers. Managing type 1 diabetes during pregnancy is often described as a full-time job, with constant vigilance required to avoid hypoglycemic (low blood sugar) or hyperglycemic (high blood sugar) episodes. The artificial pancreas alleviates this burden by automating glucose monitoring and insulin delivery, allowing women to focus on their pregnancy rather than their condition. This not only improves their quality of life but also reduces stress, which can itself contribute to better health outcomes.
The initiative is also a key component of NHS England’s Saving Babies’ Lives Care Bundle, a set of interventions aimed at reducing stillbirths, preterm births, and brain injuries. The rollout builds on previous NHS efforts, such as the universal adoption of continuous glucose monitors for women with type 1 diabetes in 2019, which was a global first. The success of that program paved the way for the current expansion of hybrid closed-loop systems, demonstrating the NHS’s commitment to leveraging technology to improve patient care.
Kate Brintworth, Chief Midwifery Officer for England, emphasizes the transformative potential of this technology, noting that it enables women with type 1 diabetes to have safer pregnancies. The ability to remotely monitor glucose levels also means fewer hospital visits, which is particularly beneficial for women managing busy lives or living far from specialized care centers. This aligns with the NHS’s broader goal of making healthcare more accessible and less invasive, ultimately improving the pregnancy experience for women with type 1 diabetes.
The long-term benefits extend beyond the pregnancy itself. As Nina Willer notes, the technology’s impact reaches families, livelihoods, and long-term health. By reducing the risk of complications during pregnancy, the artificial pancreas helps ensure healthier outcomes for both mother and baby, potentially reducing healthcare costs associated with neonatal intensive care and long-term diabetes management. Moreover, the emotional and psychological relief provided by the technology can have lasting positive effects on maternal mental health, fostering a more positive pregnancy experience and stronger family bonds.
The NHS’s decision to provide artificial pancreas systems to pregnant women with type 1 diabetes in England represents a landmark advancement in maternal healthcare. By addressing the unique challenges of managing blood glucose levels during pregnancy, this initiative promises to reduce the risks of stillbirth, miscarriage, and other complications, offering a safer and more manageable pregnancy experience.
The hybrid closed-loop system, with its ability to automate insulin delivery and allow for lower glucose targets, is a testament to the power of medical innovation to transform lives. For the 2,000 women with type 1 diabetes who become pregnant each year, this technology is more than just a medical tool—it is a lifeline that eases the physical and emotional burdens of their condition, paving the way for healthier pregnancies and brighter futures for both mothers and their babies.
This initiative also underscores the NHS’s leadership in adopting cutting-edge technology to improve patient outcomes. Building on the success of previous programs, such as the rollout of continuous glucose monitors, the NHS continues to set a global standard for diabetes care.
As more women gain access to this life-changing technology, the ripple effects will be felt not only in improved maternal and neonatal health but also in the broader societal benefits of healthier families and reduced healthcare burdens. The artificial pancreas is indeed a “game-changer,” as described by those who have experienced its benefits firsthand, and its widespread adoption marks a significant milestone in the journey toward equitable, innovative healthcare for all.

