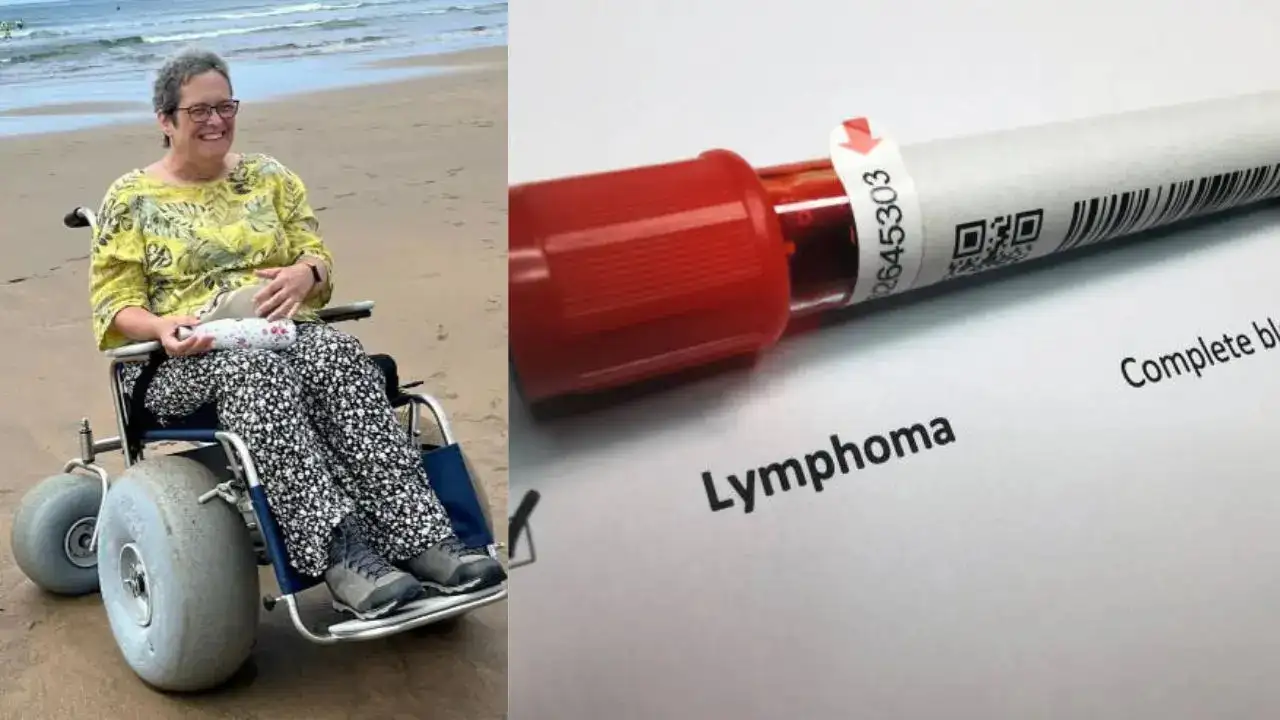
In a heartbreaking turn of events, a vibrant woman from Cornwall has been left permanently wheelchair-bound due to a delayed diagnosis of spinal cancer. Karen Davey, a 54-year-old resident of Launceston, once led an active life filled with hiking across rugged moors, cold-water swimming year-round, and even adventurous pursuits like abseiling off a 120-foot viaduct. However, what began as seemingly innocuous symptoms—hot flushes, fatigue, and a loss of appetite—escalated into a life-altering ordeal when medical professionals initially dismissed them as signs of menopause and a minor gardening injury.
This misdiagnosis allowed the cancer to progress unchecked, resulting in irreversible damage to her spinal cord. Karen’s story serves as a stark reminder of the dangers of overlooking women’s health concerns and the critical need for thorough investigations into persistent symptoms. Now in remission from stage four non-Hodgkin lymphoma, she faces a new reality marked by physical limitations, emotional turmoil, and a reliance on others for daily activities.
Her experience has propelled her to advocate for better awareness through organizations like the Spinal Injuries Association, highlighting how such oversights can devastate lives. Karen Davey’s journey underscores broader issues in healthcare, particularly for women approaching middle age, where symptoms are often attributed to hormonal changes without deeper scrutiny. As she navigates this profound change, her resilience shines through, but so does her frustration with a system that failed to act swiftly.
The Onset of Symptoms and Initial Misdiagnosis
Karen Davey’s troubles began subtly in early 2024, a time when she was still enjoying the freedoms of an independent, active lifestyle. At 54, she started noticing changes that she initially chalked up to the natural progression of menopause. Hot flushes would come and go, leaving her feeling overheated and uncomfortable. Fatigue set in, sapping her energy for the activities she loved, such as long walks in the Cornish countryside or dipping into chilly waters for a refreshing swim.
Alongside these, she experienced a gradual loss of appetite, which she tried to dismiss as part of the same transitional phase many women her age endure. By March 2024, the symptoms had intensified, evolving into something more alarming. Karen developed sharp pain in her kidneys, prompting her to seek medical advice from her general practitioner (GP). During the appointment, she described her discomfort, mentioning a recent light gardening session that lasted only about 20 minutes—well within her usual capabilities as someone accustomed to physical exertion.
To her surprise, the GP attributed the back pain solely to this minor activity, suggesting it was a simple strain from gardening. No further tests were recommended at that point, and the hot flushes and fatigue were brushed off as menopausal symptoms. Karen Davey was sent home with advice to rest and manage the pain with over-the-counter remedies. This initial dismissal proved to be a critical oversight. Over the following two months, Karen’s condition deteriorated rapidly. She stopped eating properly, leading to significant weight loss that further weakened her body.
A persistent temperature indicated an underlying infection or inflammation, but it went unaddressed in the context of her previous diagnosis. The pain in her back and kidneys persisted, but more worryingly, she began to lose sensation in her legs. Tingling in her toes gave way to numbness, and eventually, she lost control over her bladder and bowel functions. These red flags should have signaled a neurological issue, yet the connection to her earlier complaints wasn’t immediately made.
Read : LingLong Wei Sues Michigan State University for $100 Million Over Thyroid Cancer Diagnosis
Karen Davey later reflected on this period with a mix of regret and anger. She had no prior knowledge that such symptoms could point to something as severe as a spinal cord issue. “I had no idea that hot flushes would lead to all this,” she said. “The symptoms you’ve got aren’t always menopause symptoms, and we need to be more mindful of that.” Her frustration stemmed from the fact that her concerns were not taken seriously enough to warrant immediate investigation. Instead of probing deeper—perhaps with imaging scans or blood tests—her GP’s quick attribution to menopause and gardening delayed the recognition of a far more sinister cause.
Read : Large Number of Lung Cancer Patients in India Never Smoked: Lancet Study
This phase of her story highlights a common problem in women’s healthcare: the tendency to normalize or minimize symptoms associated with aging or everyday activities. For Karen, what started as manageable discomfort spiraled into a crisis that could have been mitigated with earlier intervention. By the time she was admitted to the hospital, the damage was already advancing, setting the stage for a diagnosis that would change her life forever.
The Devastating Diagnosis and Treatment
After weeks of worsening symptoms, Karen Davey’s situation reached a breaking point. She was admitted to the hospital, where she spent two grueling weeks undergoing a battery of tests. Doctors finally uncovered the true culprit: stage four non-Hodgkin lymphoma, a type of cancer that had originated in her kidneys. More alarmingly, a tumor had wrapped itself around her spinal cord, compressing vital nerves and causing the neurological deficits she was experiencing.
The diagnosis came as a shock, but it explained the cascade of symptoms that had plagued her. The hot flushes and fatigue were not merely menopausal; they were early indicators of the body’s fight against cancer. The kidney pain was directly linked to the lymphoma’s location, and the back pain—far from a gardening injury—was due to the tumor’s pressure on her spine. By the time it was detected, the cancer had advanced to a critical stage, infiltrating her spinal cord and leading to irreversible damage.
Treatment began immediately to halt the disease’s progression. Karen Davey underwent one round of radiotherapy targeted at the tumor to reduce its size and alleviate some pressure on her spine. This was followed by a course of chemotherapy to address the lymphoma systemically. The treatments were intense, taking a toll on her already weakened body, but they proved effective in combating the cancer itself. By the end of her regimen, Karen was declared in remission—a victory in the battle against the disease.

However, the remission came at a steep price. The tumor’s impact on her spinal cord resulted in permanent injury, leaving her unable to walk. Despite the cancer being under control, the neurological damage meant she could no longer feel or move her legs independently. She required extensive rehabilitation to adapt to her new circumstances, learning to use a wheelchair and managing the loss of bladder and bowel control. These changes not only affected her physically but also reshaped her daily routines and long-term plans.
Karen’s husband stepped in as her full-time carer, giving up his own work to support her through recovery and beyond. The couple’s home in Launceston had to be modified to accommodate her wheelchair, adding financial and emotional strain. Throughout this period, Karen Davey grappled with the “what ifs”—what if her symptoms had been investigated sooner? What if the gardening excuse hadn’t been accepted so readily? Her story echoes concerns raised by health advocates about diagnostic delays, particularly for conditions that mimic common ailments.
In sharing her experience, Karen Davey emphasized the need for greater awareness. “I just get annoyed that it was attributed to menopause and doing gardening when it needed looking into a bit more,” she stated. “I didn’t know anything about spinal cord injury and when my toes started going tingly, it didn’t occur to me that’s what it was. There’s not enough information.” Her treatment journey, while successful in eradicating the cancer, underscores the irreversible consequences of delayed diagnosis.
Life After Cancer: Challenges and Advocacy
Today, Karen Davey’s life looks vastly different from the one she led just a year ago. Confined to a wheelchair, she has had to scale back her professional commitments dramatically, now working only four hours a week in a role that accommodates her limitations. Simple pleasures like spontaneous outings to meet friends, browsing shops in town, or enjoying a swim are no longer feasible without assistance.
Her social life has been upended, and the emotional impact has been profound. “Emotionally, it’s just completely messed me up,” she admitted. “I’d gone from somebody who was quite active before. I’d do a lot of hiking across the moors, I used to go cold-water swimming all year round. One of the last things I did before I got ill was an abseil off a 120-foot viaduct. This isn’t what I’m supposed to be doing at this time of life.”

The dependency on her husband for everything from mobility to personal care has strained their relationship, though it has also deepened their bond. Karen is unable to drive, further isolating her in the rural setting of Cornwall. Despite these challenges, she remains determined to reclaim as much independence as possible, exploring adaptive technologies and therapies that might improve her quality of life.
Karen’s ordeal has transformed her into an advocate for change. She has partnered with the Spinal Injuries Association to raise awareness about spinal cord injuries and the importance of not dismissing women’s symptoms. The organization’s campaigns manager, Dharshana Sridhar, praised Karen’s courage, noting that her story is a “powerful reminder that women’s health symptoms should never be dismissed or explained away without proper investigation.” The association calls for better education among healthcare providers, earlier diagnostics, and more accessible care, especially for those with intersecting factors like disability.
Through her advocacy, Karen Davey hopes to prevent others from enduring similar fates. She urges women to persist if their concerns are minimized and encourages medical professionals to look beyond surface-level explanations. Her message is clear: symptoms like hot flushes or back pain deserve thorough evaluation, regardless of age or assumed causes.
In reflecting on her journey, Karen Davey’s resilience stands out amid the adversity. While the cancer is in remission, the spinal injury’s permanence serves as a daily reminder of what was lost. Yet, by sharing her story, she turns personal tragedy into a catalyst for systemic improvement, ensuring that future generations might receive the timely care she was denied.
Karen Davey’s experience is a poignant call to action in the realm of healthcare equity. It illustrates how misattributions—to menopause, gardening, or other benign causes—can lead to catastrophic outcomes. As society grapples with these issues, stories like hers pave the way for reform, fostering a more attentive and inclusive medical landscape. Though her path forward is challenging, Karen’s voice amplifies the need for change, offering hope that awareness can prevent such heart-wrenching stories in the future.