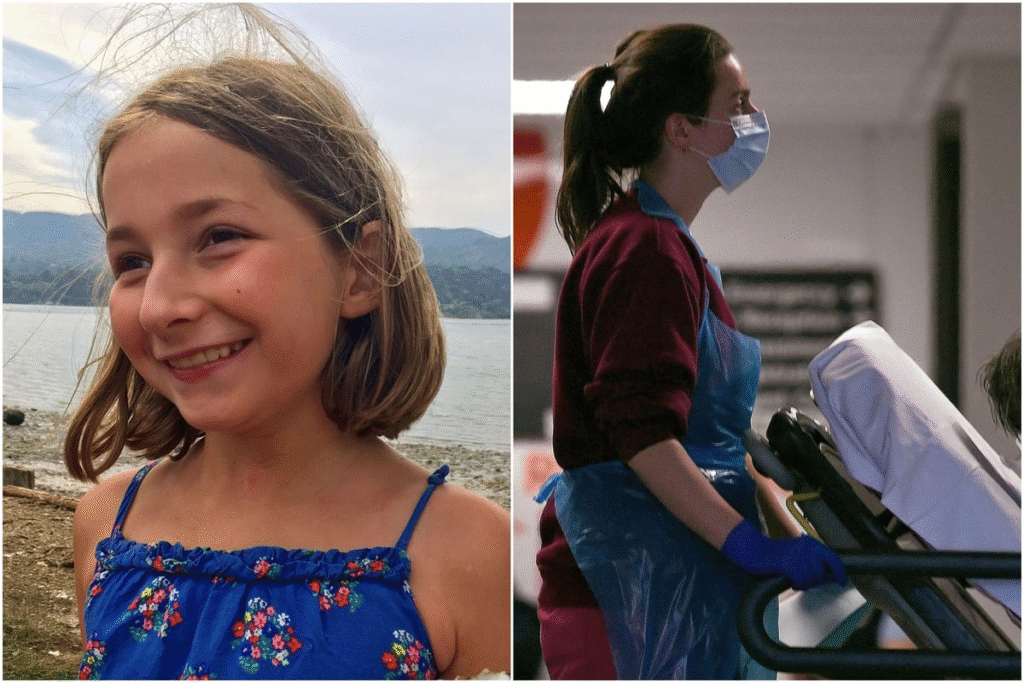
In a heartfelt campaign born from tragedy, Merope Mills, the mother of 13-year-old Martha Mills, who died of sepsis in 2021, is advocating for the expansion of Martha’s Rule to maternity care across the United Kingdom. Martha’s Rule, a patient safety initiative that allows patients and their families to request an urgent second opinion when they feel their concerns about deteriorating health are not being addressed, has already been implemented in all acute hospitals in England. The push to extend this life-saving measure to maternity services comes as a response to systemic failures in healthcare, particularly in maternity care, where families often feel dismissed or ignored.
The Tragic Loss of Martha Mills and the Birth of Martha’s Rule
Martha Mills was a vibrant 13-year-old who suffered a pancreatic injury after falling off her bike during a family holiday in Wales in 2021. Admitted to King’s College Hospital in London under the care of the paediatric liver team, Martha developed an infection that progressed into sepsis, a life-threatening condition where the body’s response to infection causes widespread inflammation and organ failure. Despite repeated concerns raised by her parents, Merope Mills and Paul Laity, about Martha’s deteriorating condition, their pleas were dismissed by medical staff.
A coroner later ruled in 2023 that Martha would likely have survived had doctors identified the warning signs of septic shock and transferred her to the intensive care unit (ICU) sooner. The failure to act on the family’s concerns was a devastating oversight. Merope Mills, a journalist and editor at The Guardian, recounted how she and her husband were “managed” rather than listened to, with symptoms like Martha’s severe bleeding and rash being misdiagnosed or downplayed.
On one occasion, a junior doctor dismissed a rash as unrelated to sepsis, and a duty consultant, who was not present at the hospital, refused to escalate Martha’s care to the ICU, citing that it would increase her mother’s anxiety. This lack of responsiveness highlighted a deep-rooted cultural issue in some hospitals, where hierarchical structures and overconfidence among medical staff can silence the voices of patients and their families.
In response to their daughter’s preventable death, Merope Mills and Paul Laity campaigned tirelessly for a system that would empower patients and families to seek urgent reviews when they feel their concerns are not being heard. This led to the creation of Martha’s Rule, which formalizes the right to request a rapid second opinion from a critical care outreach team, available 24/7, if a patient’s condition worsens.
"It's Martha's 18th birthday today… I wish beyond measure that was the thing that me and my family were celebrating today."
— BBC Radio 4 Today (@BBCr4today) September 4, 2025
Merope Mills, whose daughter Martha died of sepsis in 2021, reflects on the impact of Martha's Rule across hospitals in England.#R4Today
The initiative was inspired by similar systems, such as Ryan’s Rule in Queensland, Australia, and Call 4 Concern in some UK hospitals. Martha’s Rule was first piloted in 143 NHS hospitals in England in 2024 and, as of September 2025, is operational in all 210 acute hospitals delivering short-term treatment, with nearly 5,000 calls made to escalation helplines between September 2024 and June 2025, resulting in 720 potentially life-saving changes in care.
The Case for Extending Martha’s Rule to Maternity Care
Merope Mills’ call to extend Martha’s Rule to maternity care is driven by the recognition that women and their partners often face similar challenges in having their concerns acknowledged during pregnancy and childbirth. Speaking on BBC Radio 4’s Today programme, Mills emphasized that implementing Martha’s Rule in maternity services would give women a “greater voice” when they feel their care is inadequate. This is particularly critical in light of recent revelations about systemic failures in NHS maternity care.
In June 2025, Health Secretary Wes Streeting acknowledged that “maternity units are failing, hospitals are failing, trusts are failing, regulators are failing,” pointing to a culture of “gaslighting” families who seek answers about poor care. A 2020 investigation by The Independent and Channel 4 uncovered a decade of poor care at Nottingham University Hospital, with 46 cases of babies left with permanent brain damage, 19 stillbirths, and 15 deaths. Families reported being dismissed or accused of overreacting, echoing the experiences of Merope Mills and Paul Laity.
In June 2025, a criminal investigation into Nottingham University Hospital shifted its focus to corporate manslaughter, underscoring the severity of these failures. These incidents highlight the urgent need for a mechanism like Martha’s Rule to ensure that concerns about maternal or neonatal deterioration are taken seriously. Dr. Aidan Fowler, the national director of patient safety in England and deputy chief medical officer at the Department of Health and Social Care, has confirmed that the government is exploring options to pilot Martha’s Rule in maternity settings.

He noted that maternity care presents unique challenges, as it involves monitoring the health of both the mother and baby, as well as concerns about the progress of labor, which may require specialized expertise not always available in intensive care units. Despite these complexities, Fowler expressed support for the initiative, stating, “We do back that and we’re already looking at that.” The pilot program aims to address these challenges by ensuring that the right teams are available to respond to concerns about maternal and neonatal health.
The extension of Martha’s Rule to maternity care is seen as a vital step toward addressing the power imbalances in healthcare. Mills has argued that the initiative not only saves lives but also fosters a more equal doctor-patient relationship, where families feel empowered to challenge clinical decisions without fear of being dismissed. This cultural shift is particularly important in maternity care, where women often report feeling ignored or patronized, especially during high-risk situations like labor and delivery.
The Broader Impact of Martha’s Rule on Patient Safety
The rollout of Martha’s Rule across all acute hospitals in England has already demonstrated its potential to save lives and improve patient care. NHS England data from September 2024 to June 2025 shows that of the 4,906 calls made to Martha’s Rule helplines, 71.9% were from families, 15% from patients, and 9% from NHS staff, indicating widespread use of the system.
Approximately 2,132 calls related to acute deterioration, with 241 resulting in urgent admissions to high-dependency or intensive care units, and 720 leading to changes in care, such as the administration of antibiotics or other critical interventions. These figures underscore the importance of empowering patients and families to act as a “safety net” when clinical decisions may be inadequate.
Martha’s Rule also aligns with broader efforts to improve patient safety within the NHS. Alongside the initiative, the NHS has introduced a pediatric early warning system to track vital signs in children, building on similar systems for adults, newborns, and maternity services. This structured approach ensures that clinicians formally record changes in vital signs, such as blood pressure and heart rate, to identify deterioration early. By combining these systems with Martha’s Rule, the NHS aims to create a more responsive and patient-centered healthcare system.
The success of Martha’s Rule has prompted calls for its expansion beyond England to other parts of the UK, including Scotland, Wales, and Northern Ireland. Merope Mills has made a direct appeal to the leaders of NHS Scotland, Wales, and Northern Ireland to adopt the initiative, noting that families in these regions have expressed frustration at its absence. In Scotland, pilot programs are underway to test Martha’s Rule, with discussions about developing a nationwide approach. The initiative’s success in England, coupled with its potential to address systemic issues in maternity care, makes a compelling case for its broader adoption.
The campaign for Martha’s Rule is a testament to the resilience of Merope Mills and Paul Laity, who have turned their personal tragedy into a movement for change. On what would have been Martha’s 18th birthday in September 2025, they reflected on her absence but took solace in the fact that her legacy is saving lives. “We feel her absence every day, but at least Martha’s Rule is already preventing many families from experiencing something similar,” they said in a statement.
Their advocacy has not only highlighted the preventable nature of Martha’s death but also exposed the broader issue of epistemic injustice in healthcare, where the voices of patients and families are undervalued or ignored. As the NHS continues to grapple with challenges like workforce shortages and systemic failures, Martha’s Rule offers a practical solution to improve patient safety and rebuild trust.
Its potential extension to maternity care could be a game-changer, ensuring that women and their families have a voice in critical moments. By formalizing the right to a second opinion, Martha’s Rule challenges the culture of deference and hierarchy in medicine, paving the way for a more collaborative and responsive healthcare system. As Merope Mills continues her campaign, her message is clear: listening to patients and families is not just a courtesy—it’s a matter of life and death.

