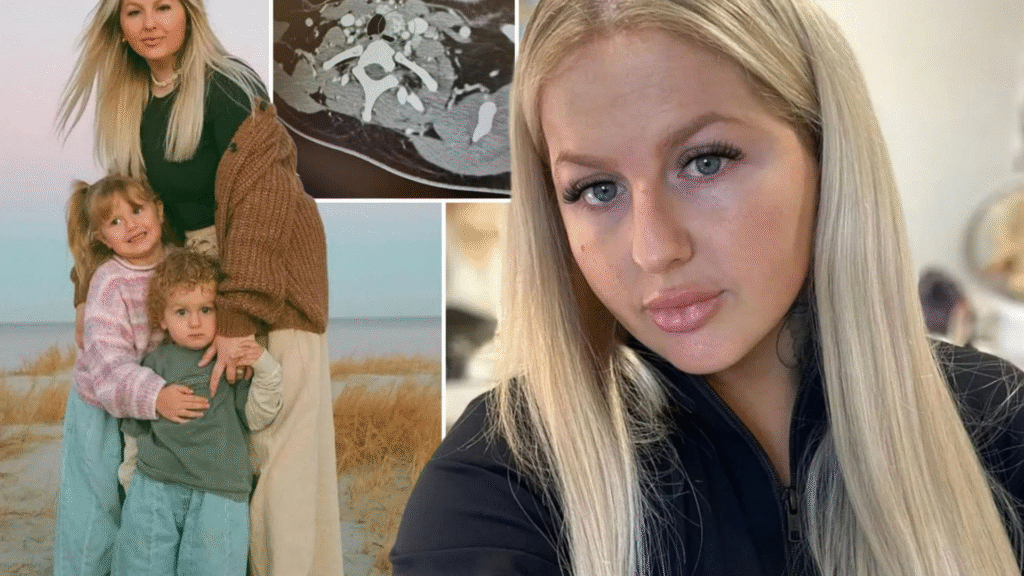
In a shocking revelation that underscores the critical need for thorough medical evaluations in postpartum women, Tameika McBride, a 30-year-old mother of two from the United States, discovered that what she and her doctors had long attributed to postpartum depression and anxiety was actually a rare and aggressive form of thyroid cancer. This story, which has recently captured widespread attention, highlights the subtle yet dangerous overlap between mental health symptoms and underlying physical conditions. McBride’s journey began innocently enough, amid the joys and challenges of new motherhood, but it quickly spiraled into a battle for her life.
Tameika McBride’s ordeal started several years ago, well before her cancer diagnosis became public knowledge. As a young mother, she welcomed her first child and later her second, a four-year-old and a two-year-old at the time of her diagnosis. Like many new parents, she experienced the emotional rollercoaster of postpartum life. However, her symptoms went beyond the typical “baby blues.”
McBride began noticing bouts of dizziness that left her unsteady on her feet, heart palpitations that made her chest feel like it was racing uncontrollably, and unexplained weight gain that seemed resistant to any efforts to manage it. These issues persisted for years, intensifying after the birth of her children. She described feeling constantly fatigued, as if an invisible weight was dragging her down, and her mood swings were severe enough to strain her daily interactions and family life.
Initially, McBride sought help from her healthcare providers, hoping for relief from what she assumed was the stress of motherhood. During her first pregnancy, she was even prescribed thyroid medication, a common intervention for hormonal imbalances that can occur during gestation. Yet, no one delved deeper into potential thyroid issues at the time. Instead, every visit to the doctor resulted in the same refrain: it was postpartum depression, anxiety, or simply her overthinking things. “Every time I went to the doctor, I was told it was postpartum depression, anxiety, or that I was just overthinking things,” McBride later shared in interviews.
She was encouraged to manage her stress through lifestyle changes, therapy, or medication for mental health, but no physical examinations of her neck or advanced imaging were recommended. This dismissal persisted despite her insistence that something felt fundamentally wrong. McBride even reflected on her childhood, believing she may have had undiagnosed thyroid problems back then, which could have allowed nodules to develop unchecked over time.
Postpartum depression, or PPD, is a serious condition affecting up to 15% of new mothers, according to medical experts. It manifests as intense feelings of sadness, irritability, and hopelessness that can interfere with bonding with the baby and daily functioning. Symptoms often include severe mood swings, frequent crying spells, fatigue, guilt, and anxiety. In McBride’s case, these emotional and psychological elements were present, but they were compounded by physical signs like the dizziness and palpitations, which are less commonly associated with pure PPD.
Heart palpitations and weight gain can sometimes be linked to anxiety disorders, but they are also hallmarks of thyroid dysfunction. The thyroid gland, a small butterfly-shaped organ in the neck, regulates metabolism, energy levels, and mood through hormone production. When it malfunctions, it can mimic mental health issues almost perfectly. The overlap between thyroid problems and postpartum depression is not uncommon. Research has shown that thyroid antibodies—proteins that can attack the thyroid— are associated with higher rates of depression during and after pregnancy.
Read : LingLong Wei Sues Michigan State University for $100 Million Over Thyroid Cancer Diagnosis
In fact, studies indicate that women with thyroid abnormalities during pregnancy have a prevalence of PPD ranging from 8.3% to 36%. Postpartum thyroiditis, an inflammation of the thyroid that occurs in the first year after childbirth, can cause hyperthyroidism (overactive thyroid) followed by hypothyroidism (underactive thyroid). Symptoms of hyperthyroidism include rapid heartbeat, anxiety, and weight loss, while hypothyroidism brings fatigue, depression, and weight gain. McBride’s symptoms aligned more with the latter, yet her thyroid levels were checked routinely without leading to scans or ultrasounds. This gap in diagnostic protocols allowed her condition to progress undetected.
Read : 100 Reasons Why Watermelon Is Your Ultimate Summer Superfood
As months turned into years, McBride’s frustration grew. She managed her symptoms as best she could, focusing on her young children and family responsibilities. But deep down, she knew there was more to her story. Social media posts from that period show her smiling for the camera, holding cakes for birthdays, but upon closer inspection, subtle clues were there. In old photos, McBride later noticed that her neck appeared different—slightly swollen or asymmetrical—indicating possible early signs of thyroid enlargement. These visual hints, overlooked at the time, would become pivotal in her eventual diagnosis. She continued advocating for herself, but the medical system seemed geared toward mental health explanations for postpartum women, a bias that can delay critical interventions.
The Turning Point: Discovery of the Swollen Lymph Node
The pivotal moment in Tameika McBride’s health journey came when she noticed a swollen lymph node in her neck. This visible lump was impossible to ignore, prompting her to demand more aggressive testing. No longer willing to accept vague reassurances, McBride pushed for a thorough investigation, including a CT scan and a fine needle biopsy. What these tests revealed was devastating: she had thyroid cancer, and it was not the garden-variety type. The biopsy confirmed cancerous cells, and further analysis showed that the disease had already spread.
This discovery happened earlier this year, marking a dramatic shift from misdiagnosis to confirmed malignancy. The swollen lymph node was a red flag that finally triggered the physical examination her neck had never received in prior visits. “I was never sent for a scan or ultrasound, and no one ever examined my neck until this year when the lymph node appeared,” McBride recounted. The CT scan provided clear images of irregularities in her thyroid, and the biopsy sealed the diagnosis. Looking back, she connected the dots: the years of symptoms were not just emotional but rooted in a physical cancer that had been brewing silently.
Thyroid cancer, while relatively rare, is the most common endocrine cancer, affecting about 12,000 women annually in the U.S. alone. It often presents with a lump in the neck, but early symptoms can be nonspecific, including fatigue, voice changes, or swallowing difficulties. In McBride’s situation, the cancer had masqueraded as mental health issues for so long because thyroid cancers can disrupt hormone production, leading to depressive symptoms.
The fact that it went undetected despite thyroid level checks highlights a key issue in medical practice: routine blood tests for thyroid-stimulating hormone (TSH) can miss structural problems like nodules or tumors unless imaging is performed. For postpartum women, this is particularly risky, as hormonal fluctuations from pregnancy can mask or exacerbate thyroid conditions.
Upon receiving the diagnosis, McBride was understandably shocked. She had spent years believing she was battling invisible demons of the mind, only to learn it was a tangible, life-threatening illness. The emotional toll was immense; she worried about her children’s future and her own survival. Yet, her determination shone through as she prepared for treatment. This turning point not only saved her life but also amplified her voice, turning her personal struggle into a public call for better healthcare awareness.
Diagnosis, Treatment, and Ongoing Battle Against Aggressive Cancer
Tameika McBride’s formal diagnosis was Diffuse Sclerosing Variant Papillary Thyroid Carcinoma, a rare and aggressive subtype of papillary thyroid cancer. This variant is characterized by diffuse involvement of one or both thyroid lobes, extensive fibrosis (scarring), dense lymphocytic infiltration, and a higher propensity for lymphatic invasion and metastasis. Unlike more common papillary thyroid cancers, which have a 98% five-year survival rate, the diffuse sclerosing variant is more challenging due to its rapid spread and resistance to standard treatments. In McBride’s case, the cancer had already metastasized to multiple lymph nodes by the time it was detected.
Treatment began promptly in April of this year with major surgery. McBride underwent a full thyroidectomy, where her entire thyroid gland was removed, along with a left modified radical neck dissection. During this procedure, surgeons excised 34 lymph nodes from her neck, of which 12 were found to be cancerous. The operation was extensive, involving careful navigation around vital structures like nerves and blood vessels to preserve her voice and mobility. Post-surgery, pathology reports confirmed the aggressive nature of the tumor, sending McBride and her medical team into high alert.
Following the surgery, McBride received radioactive iodine therapy, a standard ablation treatment for thyroid cancer. This involves ingesting a dose of radioactive iodine, which targets and destroys any remaining thyroid tissue or cancerous cells that absorb iodine. A post-treatment body scan was encouraging in some ways—it showed that two newly detected cancerous lymph nodes had absorbed the radiation, indicating potential effectiveness.

However, vigilance remains key. Doctors are monitoring her closely for any recurrence, and they have discussed the possibility of additional rounds of treatment if needed. McBride now lives without her thyroid, relying on lifelong hormone replacement therapy to regulate her metabolism and energy levels. Side effects from the surgery and radiation, such as temporary voice changes, neck stiffness, and fatigue, have been part of her recovery, but she reports steady improvement.
The aggressiveness of her cancer type adds layers of complexity to her prognosis. Diffuse sclerosing variant papillary thyroid carcinoma accounts for about 3-6% of all papillary cases and is known for its higher recurrence rate, often requiring more aggressive interventions like external beam radiation or targeted therapies in advanced stages. McBride’s case is particularly notable because the cancer’s spread to 12 lymph nodes suggests it had been present and growing for years, possibly since her childhood or early pregnancies. Early detection could have made treatment simpler, but the misattribution to postpartum depression delayed that opportunity.
Throughout her treatment, McBride has drawn strength from her family and community. Her two young children have been her motivation, and she has shared glimpses of her hospital stays and recovery on social media, holding cakes to celebrate small victories amid the hardship. Her story has resonated with many, especially mothers who have faced similar dismissals in healthcare settings.
Lessons Learned: Advocating for Thorough Checkups and Raising Awareness
Tameika McBride’s experience is a powerful lesson in the importance of holistic medical evaluations, particularly for postpartum women. What began as seemingly mental health-related symptoms—fatigue, anxiety, weight gain—turned out to be signals of a deadly cancer. This case exposes the pitfalls of over-relying on psychological explanations without ruling out physical causes. Medical guidelines recommend thyroid screening for women with postpartum depression symptoms, including blood tests and, if indicated, ultrasounds. Yet, in McBride’s interactions with doctors, these steps were insufficient, leading to a near-fatal delay.
Broader implications from her story touch on systemic issues in women’s health. Postpartum care often focuses on mental health, which is vital, but it must include comprehensive physical assessments. Studies link thyroid dysfunction to up to 36% of PPD cases, yet many providers stop at TSH levels without imaging. McBride’s advocacy emphasizes self-advocacy: patients should insist on second opinions, demand scans if symptoms persist, and track changes like neck swelling in photos. She believes her childhood thyroid issues were untreated, allowing cancer to develop, underscoring the need for lifelong monitoring in at-risk individuals.
Raising awareness about thyroid cancer’s subtle symptoms is another key takeaway. Unlike more overt cancers, thyroid issues can lurk for years, mimicking common ailments. McBride’s mission now is to empower others, especially mothers, to speak up. Her story has sparked discussions on social media and in health forums, encouraging women to examine their necks regularly and question dismissals. As she continues monitoring for recurrence, McBride remains optimistic, focusing on her children’s milestones and her role as a survivor.
In conclusion, Tameika McBride’s transformation from a misdiagnosed mother to a cancer warrior is both heartbreaking and inspiring. Her case reminds us that health is interconnected—mental and physical symptoms demand integrated care. By sharing her truth, McBride is not just healing herself but potentially saving lives. As awareness grows, we hope for changes in postpartum protocols, ensuring no one else endures what she did. This story, unfolding in real time, continues to evolve, but one thing is clear: persistence pays off.

